If you are interested in empowering others to address common payment issues, we are eager for you to join us!
The APTA RI Payment Committee meets once a month on Tuesday evenings.
Email Yvonne Swanson if interested
The APTA RI Payment Committee has developed a useful document and patient letter template to help with these issues.
We’re proud to share a significant advocacy win led by the APTA Rhode Island Payment Policy Committee!
As a direct result of persistent engagement and follow-up, Neighborhood Health Plan of Rhode Island (NHP-RI) has confirmed adoption of the updated 2025 Medicaid reimbursement rates.
This action was prompted by APTA RI’s identification of NHP’s obligation—as a Medicaid Managed Care Organization—to comply with state-mandated rates, a requirement that had gone unrecognized until our intervention.
NHP will be notifying Medicaid network PT providers
Six key CPT codes have received notable increases. 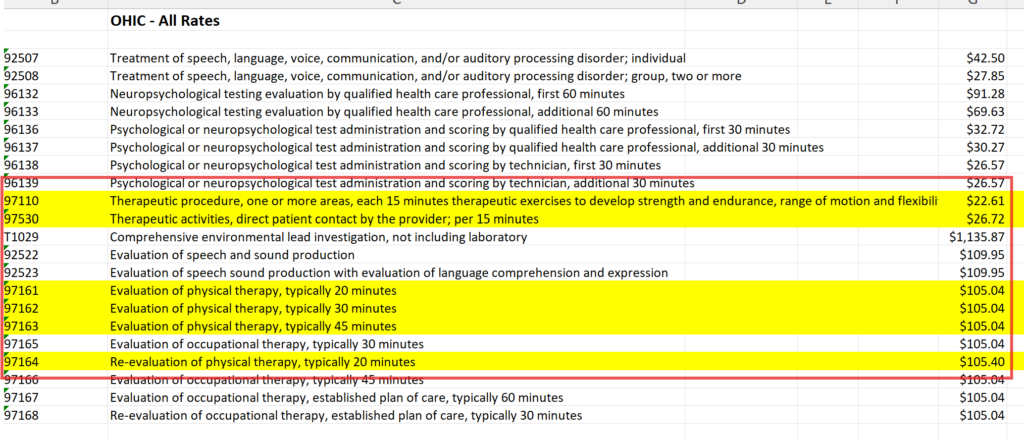
Rate increase is effective retroactively to October 1, 2024.
Any code paid less than the FFS rates will be increased to align with the revised rates.
NHP will update Medicaid fee schedules for system implementation within 45 days.
No action is needed now, but providers should monitor remits and contact NHP with any questions.
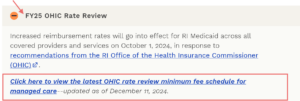
Link to Executive Office of HSS re Medicaid Reimbursement Rates. Scroll down the FY25 Rate review tab and click the link for OHIC Rate review for MCO highlighted in red below.
![]() This outcome ensures improved reimbursement for physical therapy providers across the state, and strengthens access to care for our Medicaid patient population.
This outcome ensures improved reimbursement for physical therapy providers across the state, and strengthens access to care for our Medicaid patient population.
APTA RI working for you!
March 2025: Telehealth
APTA RI Advocacy Update: Telehealth Under Medicare
July 2024 APTA State Payment Forum
Yvonne Swanson represented APTA RI at this forum in Kansas City.
Click here for the powerpoint during the forum.
June 2024
Collecting Data on the Impact of NHP’s prior authorization – please help
Neighborhood Health Plan of Rhode Island’s recent decision to add prior authorization and utilization management practices to PT, OT and SLP has greatly impacted providers and practices. The APTA RI Payment Committee would like to collect data that tracks administrative burden on clinical and administrative teams to use in future advocacy regarding this decision. Please consider having your team complete this. To also make an impact, ask your patients affected by this to send a letter to NHP.
Please find attached 2 important documents from the Payment Committee to support all Providers and Practices impacted by NHP’s decision to add prior authorization and utilization management practices to PT, OT and SLP.
May 2024
Effective June 1st, NHP will require prior authorization (PA) for PT/OT/Speech services:
As most of you know, PT/OT/Speech are being required to secure prior authorization (PA) under a new policy adopted by NHP utilizing Evolent Health as the administrator. Despite our advocacy efforts underscoring the value of rehab services and total cost of care savings, NHP’s decision stands.
To ensure readiness, NHP has announced Provider Training Sessions via Evolent Health on May 22nd, 24th, and 30th specifically for the Physical Medicine Provider group. Meeting details listed here.
APTA RI is urging all impacted providers to:
While we don’t believe PA is necessary and the increased administrative burden has a significant impact on practices, it is critical that therapists understand how NHP’s PA system will work for not only a smooth transition, but to ensure our concerns are built on a solid foundation of provider knowledge on the new policy rules.
Additionally, APTA RI advises practices to PLEASE monitor their experiences with Evolent and prior authorization as this policy rolls out. For any inquiries or assistance, please don’t hesitate to contact Yvonne Swanson.
April 2024
Adapted from March 22, 2024 APTA Friday Focus – Payment:
Providers and patients continue to deal with the effects of the massive Feb. 21 cyberattack, the largest health care hack to date. Here’s a roundup of useful information, including links to Change and UnitedHealth resources, HHS announcements, media coverage, and more.
After putting the move on hold for three months, the insurer implemented the reduction March 1.
Spending Deal Reached: Includes Some Relief From Fee Schedule Cuts
The package includes a 1.68% boost to the fee schedule but falls short of totally eliminating the cut to dozens of providers
From APTA Magazine: Direct-to-employer physical therapy companies take out the insurance middleman.
February 2024
NHP partnered with Evolent Health to manage services for PT, OT, SLP through National Imaging Associates (NIA)
Review of Policy Key Points:
Want help calculating Medicare payments? …APTA’s Fee Schedule Calculator for 2024 is now available!
2024 Fee Schedule Calculator Now Available to APTA Members
“Great tool that’s easy to use!”
Reflects where payment stands as of Jan. 19th. If Congress makes changes, the tool will be updated.
Medicare Physician Fee Schedule cuts of 3.4% continue….We need your help TODAY!
Congress kicked the can down the road in January giving ALL stakeholders more time to voice their concerns to local legislators about the impact of these cuts.
Support H.R. 6683 through the APTA Patient Action Center or Legislative Action Center. It’s fast and easy!
November 2023
Local Payor Updates:
Huge win! Blue Cross Blue Shield Increases max allowable per visit! : Sign in to your BX account for detailed description
Blue Cross Blue Shield Removes referral requirements effective Jan. 1st 2024 for PT and OT services under the following products:
Summary of CMS’ Physician Fee schedule and final rule adapted from APTA 2024 PFS and Final Rule update
October 2023
APTA RI Payment Committee
APTA RI has an active Payment Committee. This committee advocates for local payment issues and monitors important federal issues to share with members.
Recently this committee advocated against NHP’s Integrity policy shift to a 24 visit cap. The appeal has resulted in reversal!
This reversal improves access to care by eliminating the cap and arduous process of appeal while maintaining the initial 24 visits before prior authorization is required.

Adapted from APTA Friday Payment Focus:
The Proposed ’24 Fee Schedule: Takeaways From APTA’s Comments to CMS
APTA seized the opportunity to address the good, the bad, and the unclear.
Aetna Will Adopt PTA Pay Differential
The 15% reduction, set to begin Dec. 1, would mimic CMS cuts adopted in 2022. APTA is pressing Aetna to reconsider.
CMS Enters New Territory, Proposes Staffing Requirements for LTC Facilities
Most nursing homes would fall short of the requirements, which also include more detailed facility assessments and a constant RN presence.
The contact for this committee is Yvonne Swanson
July 2023
April 2023
Navigating Insurance – APTA RI Payment Committee Tips for success:
Adapted from APTA’s Friday Focus: Remote Therapeutic Monitoring: APTA Updates
Cigna
On 3/2/23 APTA met with Cigna leadership. These meetings will be held 2x a year with the next in fall 2023. ASH leadership also joined at the suggestion of Cigna. Highlights are noted below:
Discussed PT in prevention and wellness including the annua visit. Cigna relayed that coverage is benefit driven and both ASH and Cigna asked if there was evidence demonstrating that the annual visit is cost effective? There is currently no evidence and or expressed interest in implementing or conducting a pilot to collect data.
Cigna is primarily involved with surgical value-based models that extend from admission to hospital discharge. Possibly in the future they may consider include pre/post op PT, but no plans are imminent.
Both ASH and Cigna expressed support for continued remote services. Cigna: is looking at all aspects of telehealth including Remote Physiological Monitoring.
NIA/Magellan
National Imaging Associates: Physical Medicine – Guideline Pending – High Importance Update
Issued a new version of the document. Review date: 07/01/2023. Next review date (est.): 07/01/2024
View Full Policy – PDF View Full Policy – Payer Website
UHC
Upon a change in the UHC association leadership team, the meetings were postponed until the new staff was on boarded. The next meeting is currently planned for June 2023.
ASH- American Specialty Health
ASH Newsletter: https://www.ashlink.com/ash/WCMGenerated/JanFeb2023_RS_online_tcm17-213294.pdf
AIM
In March 2023, AIM Specialty Health® transitioned to Carelon Medical Benefits Management Inc. Per Anthem, “This transition is a name change only, and there will be no process changes”. If providers inquire, please let them know to check their February 2023 Anthem newsletter for the announcement. Here is info found during a google search.
SecureCare (SC)
On 3/21 APTA and the pay chairs from MN and MI met to discuss the status of the SC implementations in their state. On 3/28 APTA met with SC to review the rehab program.
Additional Resources:
Prior Auth
January 2023
Neighborhood Health Plan -Integrity: Removed Prior Authorization requirement for PT and OT beyond 24 sessions per calendar year for INTEGRITY members, effective Jan. 1st 2023
More information: Physical-and-Occupational-Rehabilitation-Services-eff-1.01.23.pdf
ASH-American Specialty Health
New clinical guidelines were issued at the end of the year and can be found here
Article:
CMS rule aimed at improving Medicare Advantage draws praise | Healthcare Dive
Payment Resources:
State Payer Advocacy Resource Center (SPARC):
A joint initiative of payer resources brought to you by APTA and APTA Private Practice Section
Website Design and Digital Marketing by